By Ben Tzeel
Children with Diabetes is an amazing conference for a variety of reasons. You can read more about how they unite kids and families living with diabetes from around the world in my previous post here. Beyond that, they offer a ton of great educational sessions, on a wide range of diabetes topics including…
…adventure? When I heard that, I was surprised and intrigued.
As I walked into the room for the talk led by Peter Nerothin, a fellow type 1 and outdoor researcher, I saw a number of parents in the room. Later, during the group activity I learned many had newly diagnosed children.
Peter’s presentation, “Everyday Management of T1D Through the Lens of Adventure,” really opened my mind to a whole new world of possibilities and reasons for why challenging ourselves can help us live our best life.

Diabetes is an adventure.
Peter shared that an adventure, by definition, is the risky undertaking of an uncertain outcome.
Uncertainty can be scary….
…but uncertainty is where we GROW and how we move ahead in life.
Living with diabetes, there is plenty of uncertainty floating around our minds at all times:
“How many grams of carbs are in this food?”
“Will this exercise make my blood sugar crash?”
“How much insulin do I need as a correction for this blood sugar?”
And facing this uncertainty, your options are to play “sit it out” or play to “win and grow.”
In both contexts, you can (and should) apply your previous experience to a situation.
But in the former option, you may stunt your growth, while in the latter, you are promoting your growth.
It’s scary at times. But at the same time, you need to ask yourself where sitting out will get you, both in your diabetes management and in life.
Will you do the things you’ve always wanted to do?
Will you experience the foods that you always have wanted to try and enjoy the foods that you love?
Will you get to be as active as you want?
Most importantly: Will you live your best life?
Peter mentioned an outdoor program for youth that informs parents that “no, we cannot guarantee the safety of your child.”
Sounds crazy, right? Hearing the statement, the parents in the conference room were unsure about whether they would send their child with diabetes to that camp.
But the facilitators’ rationale is: if you can guarantee safety, the program isn’t worth running.
The one way to guarantee safety is to leave a child in their room all day and never expose them to the outside world.
Is that child living their best life?
Risk is an essential part of life, spanning from outdoor adventure to diabetes management, and the two go hand in hand, according to Peter.
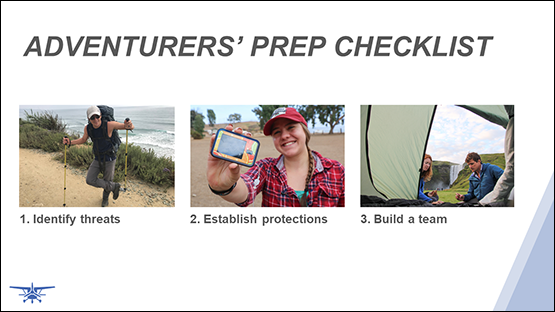
Imagine you are going on a hiking expedition. Are you going to just start on the trail without any prior preparation? Or are you going to survey the trail, gather data, develop a strategy, ensure you have supplies, backup supplies, and backups to the backups?
(Hopefully you chose the latter option).
You’re going to prepare, obviously. You’re going to determine your starting point, what provisions you will need, what obstacles you could face, and how you will overcome said obstacles with a protection plan.
This mirrors diabetes management almost to a T.
I’m a registered dietitian, so I relate a lot of things to food. Think about it:
You decide to go to a restaurant to eat with your friends. There’s a dessert on the menu that you have been DYING to try.
You have three legitimate options, two involving risk:
- You avoid the dessert (no risk)
- You eat, dose insulin, and pray (risk)
- You gather information for a starting point, consider your insulin situation (insulin-on-board, starting blood sugar), determine nutrition information, consider what will happen in case your insulin dose is not spot on, and dose insulin (risk).
Reading this example, it seems obvious which you would choose…
But you would not believe the number of individuals who choose #1…because they are afraid.
They are afraid of taking the risk due to the possible repercussions that could follow. But really, they are perfectly capable of executing on option #3.
Nerothin, Peter. “Everyday Management of T1D Through the Lens of Adventure.” July 18, 2019. Children with Diabetes, Orlando, FL.
You could replace the dessert context in the example above with beginning physical activity or with trying new diabetes technology, and it would remain true.
People will go to the ends of the earth to avoid change, risk, and discomfort, even when they know there is the potential to benefit from the change. That benefit could be as simple as full heartedly enjoying a dessert, reducing the burden of their diabetes with a new tool, or experiencing the beauty of a remote natural spot, and it still spooks them.
Why? Because people are afraid of failing at something different or new.
But they need to recognize there is a MAJOR difference between failing because of a lack of preparation and failing while being prepared.
When you are prepared you may run into minor roadblocks; like an infusion site failure on a hike. If you have backup supplies, it’s a nuisance, but not a crisis.
Failing while being prepared is known as reference experience, which can be applied to the future.
When you reframe failure as learning, suddenly, it doesn’t seem quite as scary…and the only way to improve at something is to DO IT.

Ben Tzeel, hiking in Highlands, NC.
As you become more skilled at something, the lesser the perceived risk, the less scary it becomes until eventually, it’s no longer perceived as a risk at all.
With diabetes, nothing is going to be perfect all the time. You could eat the same meal at the same time with the same insulin and the same starting blood sugar, three days in a row and end up with three very different results.
But, continuing to try new things, continuing to expand your horizons, to take risks, and to remain open minded is where the growth and development are going to happen in your life.
For example, one of the scenarios Peter encouraged participants to consider was a child’s first sleepover. A parent in the breakout group shared how the scenario related to her family; they’d avoided sleepovers because she was terrified, but her child wanted to go.
…this was answered with some strategies from other members of the group who had experience in this area, and as she learned how others prepared for the activity the mother relaxed and realized, “you know what? It’s going to be ok.”
It’s amazing how having a plan and a support team to help you execute it can make all the difference.
But, remember to retool as needed as more intel is acquired….and the most important thing?
We get stronger when faced with adversity, so don’t stop the adventure.
Peter Nerothin’s participation at the 2019 Children with Diabetes Conference was courtesy of Tandem Diabetes Care.
Author Bio: Ben Tzeel has lived with type 1 diabetes since 1999. He has a master’s degree in nutrition from the University of North Carolina at Chapel Hill and is a registered dietitian. He is a Certified Strength and Conditioning Specialist (CSCS) through the National Strength and Conditioning Association, is a published fitness model, and writes about exercise and nutrition.
Ben Tzeel was compensated by Tandem Diabetes Care for his contribution on this topic. However, he created the content and it is based on his personal knowledge, experiences, and observations.
Federal (USA) law restricts the t:slim X2 insulin pump to sale by or on the order of a physician. The t:slim X2 insulin pump with interoperable technology is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in persons requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally-connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The pump is indicated for use with NovoLog/NovoRapid or Humalog U-100 insulin. The pump is indicated for use single patient use in persons six years of age and greater. The pump is not intended for anyone unable or unwilling to: use the insulin pump, CGM, and all other system components in accordance with their respective instructions for use; test blood glucose levels as recommended by their healthcare provider; demonstrate adequate carb-counting skills; maintain sufficient diabetes self-care skills; see their healthcare provider regularly. The user must also have adequate vision and/or hearing to recognize all functions of the pump, including alerts.
From time to time, we may pass along: suggestions, tips, or information about other Tandem Insulin Pump user experiences or approaches to the management of diabetes. However, please note individual symptoms, situations, circumstances and results may vary. Please consult your physician or qualified health care provider regarding your condition and appropriate medical treatment. Please read the Important Safety Information linked below before using a Tandem Diabetes Care product.